Strategic grant
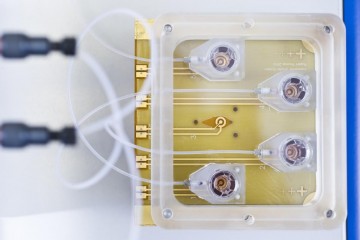
A tissue engineered construct to monitor mucosal immunity in asthma
At a glance
Completed
Award date
January 2011 - March 2014
Grant amount
£499,713
Principal investigator
Professor Donna Davies
Co-investigator(s)
Institute
University of Southampton
R
- Replacement